ACA 2025: Subsidies, Eligibility, and Your Health Coverage

The Affordable Care Act (ACA) will see notable changes in 2025 regarding subsidies and eligibility, directly influencing healthcare affordability and access for millions of Americans.
As we approach 2025, a critical look at the evolving landscape of healthcare in the United States becomes essential. The ACA 2025 Subsidies and eligibility criteria are poised for significant adjustments, directly impacting how millions of Americans access and afford health insurance.
Understanding the Affordable Care Act (ACA) Landscape
The Affordable Care Act, often referred to as Obamacare, revolutionized the U.S. healthcare system by expanding health insurance coverage. Enacted in 2010, its primary goals included making health insurance affordable, expanding Medicaid, and supporting innovative medical care delivery methods. For many, the ACA has been a lifeline, offering access to essential health benefits and financial assistance through subsidies.
The foundation of the ACA rests on several key pillars designed to broaden coverage. These include the individual mandate (though largely nullified), the creation of health insurance marketplaces (exchanges), and provisions for premium tax credits and cost-sharing reductions. Understanding these core components is crucial to grasping the implications of any future changes.
The Role of Marketplaces and Subsidies
Health insurance marketplaces are central to the ACA’s structure, serving as platforms where individuals and families can compare and purchase health insurance plans. These marketplaces are where eligible individuals can also apply for financial assistance, which comes in two primary forms: premium tax credits and cost-sharing reductions.
- Premium Tax Credits (Subsidies): These are refundable credits that lower your monthly health insurance premium payments. Eligibility is primarily based on income relative to the federal poverty level (FPL) and household size.
- Cost-Sharing Reductions (CSRs): These reduce the amount you have to pay for deductibles, copayments, and coinsurance. CSRs are available to individuals and families with incomes below 250% of the FPL who enroll in a Silver-level plan.
- Expanded Medicaid: The ACA also allowed states to expand their Medicaid programs to cover more low-income adults, significantly increasing access to care for vulnerable populations.
The ongoing evolution of the ACA means that its provisions are subject to review and modification. As we look towards 2025, it’s vital for consumers, policymakers, and healthcare providers to stay informed about potential shifts in these foundational elements, especially concerning financial aid.
Key Changes to ACA Subsidies in 2025
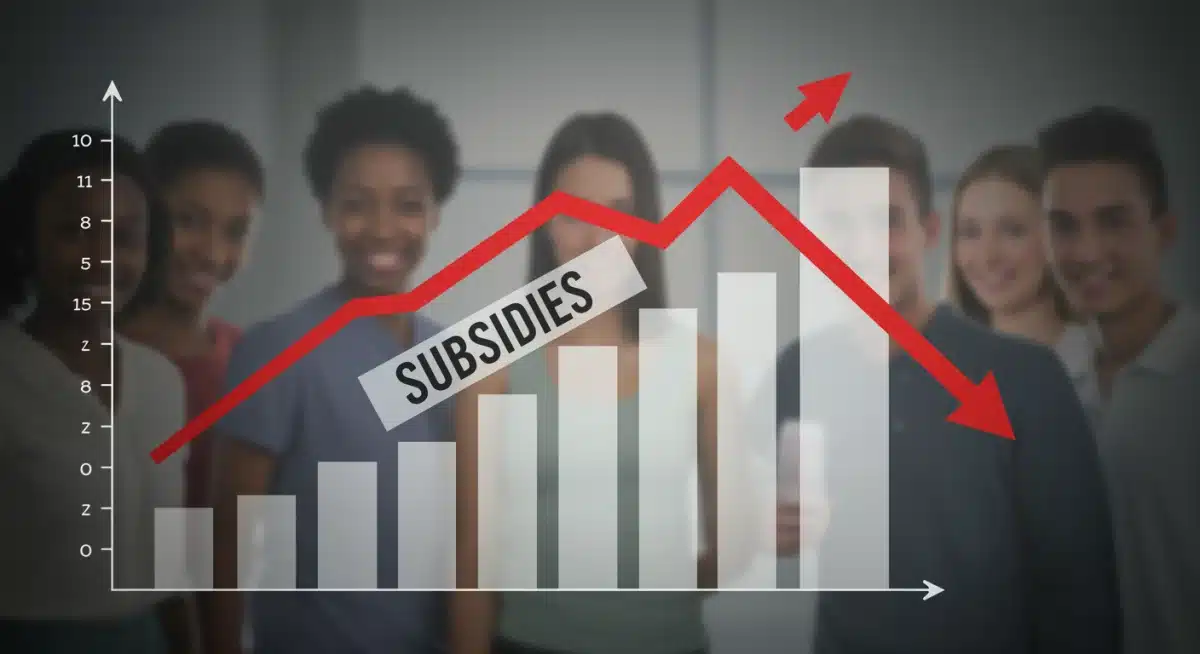
The landscape of ACA subsidies is not static; it has seen various adjustments since its inception, with significant enhancements made by the American Rescue Plan Act (ARPA) in 2021 and extended by the Inflation Reduction Act (IRA) in 2022. As these temporary enhancements are set to expire at the end of 2025, understanding the impending changes is paramount for current and prospective enrollees.
Specifically, the enhanced subsidies, which made coverage significantly more affordable for many, are slated to revert to their pre-ARPA levels. This means that without further legislative action, individuals and families will likely face higher premium costs starting in January 2026 for their 2025 coverage.
Impact of Expiring Enhanced Subsidies
The temporary subsidy enhancements eliminated the “subsidy cliff,” which previously meant individuals earning over 400% of the Federal Poverty Level (FPL) were ineligible for any premium tax credits. Under the enhancements, no one paid more than 8.5% of their household income for a benchmark Silver plan, regardless of income. The expiration of these provisions will reintroduce this income cap.
- Increased Premium Costs: Many individuals and families, particularly those with incomes above 400% FPL, will see a substantial increase in their monthly premium payments.
- Return of the “Subsidy Cliff”: The re-establishment of the 400% FPL income threshold for subsidy eligibility could leave middle-income earners without financial assistance, making health insurance unaffordable for some.
- Reduced Enrollment: Higher costs could potentially lead to a decrease in marketplace enrollment as some individuals may find coverage too expensive without the enhanced support.
These changes are not merely administrative; they have tangible financial implications for millions of Americans who rely on the ACA for their health coverage. Awareness and proactive planning will be crucial to navigating these shifts effectively.
Eligibility Criteria for ACA Subsidies in 2025
Eligibility for ACA subsidies has always been tied to a combination of factors, primarily income level, household size, and access to other affordable coverage. With the anticipated changes in 2025, these criteria will become even more critical for individuals seeking financial assistance.
The primary determinant for receiving premium tax credits is household income relative to the Federal Poverty Level (FPL). Historically, subsidies were available to those with incomes between 100% and 400% of the FPL. The enhanced subsidies temporarily removed the 400% cap, but its return will significantly alter who qualifies for assistance.
Understanding Income Thresholds
The FPL is annually updated by the Department of Health and Human Services. For 2025, these figures will define the boundaries of subsidy eligibility. Individuals and families must accurately estimate their modified adjusted gross income (MAGI) to determine where they fall within these percentages.
- 100%-400% FPL: Individuals within this income bracket are typically eligible for premium tax credits, with the amount of subsidy decreasing as income approaches the 400% mark.
- Below 100% FPL: In states that have expanded Medicaid, individuals below 138% FPL are usually eligible for Medicaid. In non-expansion states, this group may fall into a “coverage gap” and not qualify for either Medicaid or marketplace subsidies.
- Above 400% FPL: Post-2025, individuals above this threshold will likely not be eligible for premium tax credits, unless further legislative action extends the enhanced subsidies.
It’s also important to note the “family glitch,” which affects individuals who have an offer of employer-sponsored coverage deemed affordable for the employee only, but not for the entire family. While the Biden administration addressed this issue, it remains a complex area for subsidy eligibility. As 2025 approaches, individuals should review their eligibility carefully, considering all household income sources and family configurations to ensure they maximize any available financial assistance.

Navigating the Health Insurance Marketplace for 2025 Enrollment
Enrolling in a health insurance plan through the marketplace can seem daunting, but understanding the process is key to securing affordable and comprehensive coverage. For 2025, with potential changes to subsidies, careful navigation of the marketplace becomes even more crucial.
The annual Open Enrollment Period (OEP) is the primary time to enroll in a new plan or change existing coverage. Outside of OEP, a Special Enrollment Period (SEP) may be available for individuals experiencing qualifying life events such as marriage, birth, loss of other coverage, or moving.
Steps for a Successful Enrollment
The enrollment process typically involves several steps, from creating an account to selecting a plan. It’s advisable to start early, gather necessary documents, and compare plans thoroughly to find the best fit for your needs and budget.
- Create or Update an Account: Begin by visiting HealthCare.gov or your state’s health insurance marketplace website to create an account or log in to an existing one.
- Estimate Your Income: Accurately project your household income for 2025. This is vital for determining your subsidy eligibility and the amount of financial assistance you may receive.
- Compare Plans: Utilize the marketplace tools to compare different plans based on premiums, deductibles, out-of-pocket maximums, and covered services. Pay attention to plan categories (Bronze, Silver, Gold, Platinum).
- Seek Assistance: If you find the process confusing, free assistance is available from navigators, certified application counselors, and licensed insurance agents.
Remember that even if you’re currently enrolled, it’s wise to re-evaluate your options each year. Plan offerings and your personal circumstances can change, and what was the best plan last year might not be the most suitable for 2025, especially with the impending subsidy adjustments.
Potential Impact on Healthcare Costs and Access
The anticipated changes to ACA subsidies in 2025 are expected to have a multifaceted impact on healthcare costs and access across the United States. For millions of Americans, particularly those who benefited most from the enhanced subsidies, the financial burden of health insurance could increase significantly.
Higher premiums and out-of-pocket costs could lead to difficult choices for families and individuals. Some may opt for less comprehensive plans, delay necessary medical care, or, in extreme cases, forgo health insurance altogether, increasing the rate of uninsured individuals.
Disproportionate Effects on Vulnerable Populations
The impact is unlikely to be evenly distributed. Vulnerable populations, including low-to-moderate income families, self-employed individuals, and those in states that have not expanded Medicaid, may face the greatest challenges.
- Reduced Affordability: Without the enhanced subsidies, the cost of benchmark plans could become prohibitive for many, pushing health insurance out of reach.
- Increased Uninsured Rates: A rise in costs often correlates with an increase in the number of uninsured Americans, leading to poorer health outcomes and greater reliance on emergency care.
- Strain on Healthcare Providers: A higher uninsured rate can also strain healthcare providers, who may face an increase in uncompensated care.
Conversely, continued advocacy and potential legislative efforts could emerge to extend or modify the enhanced subsidies, mitigating some of these anticipated negative impacts. The ongoing debate highlights the critical role of policy decisions in shaping the nation’s healthcare landscape and ensuring equitable access to care for all citizens.
Advocacy and Future Outlook for ACA Reforms
The discussion around ACA 2025 Subsidies and eligibility is not merely about policy; it’s about the health and financial well-being of millions of Americans. As the expiration of enhanced subsidies looms, advocacy groups, policymakers, and healthcare stakeholders are actively engaged in discussions about the future of the Affordable Care Act.
There is a strong push from various organizations to make the enhanced subsidies permanent. Proponents argue that maintaining these subsidies is essential for preserving the gains in coverage achieved under the ACA and preventing a surge in uninsured rates. They emphasize the economic stability and improved public health outcomes that come with broader health insurance access.
Legislative Efforts and Public Pressure
The legislative calendar for 2024 and 2025 will be critical in determining the fate of these subsidies. Congressional action would be required to extend the enhanced premium tax credits beyond their current expiration date. Public pressure and constituent feedback will undoubtedly play a significant role in influencing these political decisions.
- Congressional Debates: Expect robust debates in Congress regarding the affordability of healthcare and the role of government subsidies.
- Advocacy Campaigns: Consumer advocacy groups, healthcare organizations, and patient groups will likely launch campaigns to highlight the importance of affordable coverage.
- Economic Arguments: Arguments will center on the economic impact of both extending and allowing the subsidies to expire, considering effects on household budgets, state healthcare systems, and the broader economy.
While the future remains uncertain, the dialogue surrounding ACA reforms underscores the ongoing commitment to ensuring that healthcare remains accessible and affordable. Individuals and families should stay informed about these developments, as legislative outcomes will directly shape their healthcare options in the years to come.
Preparing for 2025: Steps for Consumers
Given the potential shifts in ACA 2025 Subsidies and eligibility, proactive preparation is crucial for consumers. Taking the right steps now can help you navigate the upcoming changes and ensure you maintain affordable health coverage.
The first and most important step is to stay informed. Regularly check official government websites like HealthCare.gov and reputable news sources for updates on legislative actions and policy changes. Understanding the rules as they evolve will empower you to make informed decisions about your health insurance.
Practical Tips for Navigating Changes
Beyond staying informed, there are several practical actions you can take to prepare for the 2025 enrollment period and beyond. These steps focus on financial planning, exploring all available options, and seeking expert guidance.
- Review Your Current Plan: Understand your current plan’s benefits, costs, and how it would change if subsidies are reduced. This baseline knowledge is essential for comparison.
- Estimate Your 2025 Income: Accurately projecting your household income for the upcoming year is critical for determining your eligibility for any remaining subsidies or other financial aid.
- Explore All Options: Don’t limit yourself to just marketplace plans. Investigate employer-sponsored coverage, Medicaid, or CHIP if you might qualify.
- Consult with Experts: Utilize the free assistance offered by marketplace navigators, certified application counselors, or licensed insurance agents. They can provide personalized advice and help you understand complex eligibility rules.
- Budget for Potential Increases: If you anticipate higher premiums, begin to adjust your household budget accordingly to accommodate potential increases in healthcare costs.
By taking these proactive measures, consumers can better position themselves to adapt to the 2025 changes, minimizing potential disruptions to their healthcare access and financial stability. The goal is to ensure continuous, affordable coverage, even as the regulatory environment shifts.
| Key Point | Brief Description |
|---|---|
| Enhanced Subsidies Expiry | Temporary ACA subsidy enhancements from ARPA and IRA are set to expire at the end of 2025, potentially increasing premiums. |
| Income Cap Reinstatement | The 400% FPL income cap for subsidy eligibility is expected to return, impacting middle-income earners significantly. |
| Open Enrollment Importance | Thorough review and comparison of plans during the 2025 Open Enrollment Period will be critical for securing affordable coverage. |
| Proactive Consumer Steps | Consumers should estimate income, explore all options, and seek expert advice to prepare for potential cost increases. |
Frequently Asked Questions About 2025 ACA Changes
The primary change is the expiration of enhanced subsidies introduced by ARPA and IRA. This means the 400% Federal Poverty Level (FPL) income cap for eligibility will likely return, leading to higher premiums for many, especially those with incomes above this threshold.
Middle-income individuals and families earning above 400% of the FPL will likely be most affected, as they may lose access to premium tax credits. Additionally, those who saw significant premium reductions due to the temporary enhancements will face increased costs.
Eligibility is based primarily on your estimated household income for 2025 relative to the Federal Poverty Level (FPL) and your household size. You can use tools on HealthCare.gov or consult with a marketplace navigator to get a personalized assessment.
During the 2025 Open Enrollment Period, it is crucial to re-evaluate your health insurance options. Compare plans, accurately estimate your income, and consider seeking help from certified counselors to ensure you select the most affordable and suitable coverage.
Yes, many advocacy groups and some policymakers are actively working to make the enhanced ACA subsidies permanent. However, this would require new legislative action by Congress, and the outcome remains subject to ongoing political debates and negotiations.
Conclusion
The anticipated changes to ACA 2025 Subsidies and eligibility represent a pivotal moment for healthcare affordability in the United States. As temporary enhancements are set to expire, millions of Americans face the prospect of increased health insurance costs. Understanding these shifts, proactively planning, and engaging with available resources will be paramount for individuals and families to navigate the updated landscape successfully and maintain access to essential healthcare coverage.